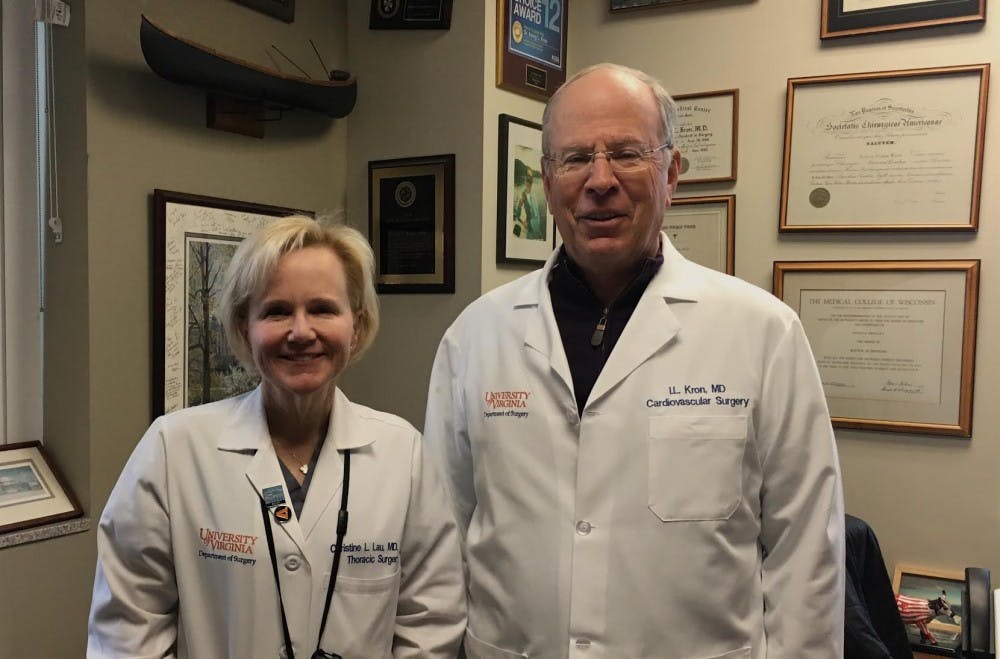
After conducting 20 years of research, doctors at the University have begun testing a lung transplant drug on humans. Surgery professors and certified thoracic surgeons Christine Lau and Irving Kron, lead researchers of the study, recently initiated phase one, or a “safety trial,” to determine the safest drug dosage to administer to patients during surgery. The investigated drug, called regadenoson, is expected to increase success rates of lung transplants.
According to Kron, the beginning of this trial dates back 20 years to a dinner conversation between himself and Dr. Joel Linden, a former physiologist at the Medical Center. The two were discussing possibly testing the medication regadenoson as a vasodilator — a drug that dilates or opens up blood vessels — to enhance medical imaging. During the exchange, Kron offered to test Linden’s Regadenoson in his research lab.
“That developed basically a 20 year long collaboration,” Kron said. “So, it basically happened when I was sitting next to [Joel Linden] and talking about mutual interests.”
After analyzing the drug in his lab, Kron noticed that regadenoson also treats inflammation, the body’s automatic immune response to a stimulus it perceives as harmful. This uncontrollable response causes redness, swelling, pain, loss of function and increases the blood flow to the inflamed area of the body.
“It turns out all of these drugs have multiple things they can do,” Kron said. “It works in imaging because it causes dilation of the blood vessels … but it also has a very direct effect on the white blood cells that cause injury.”
By understanding the properties of regadenoson and recalling a past surgery, Kron realized it could be used to treat inflammation during lung transplantation.
“In terms of the clinical situation, I started a lung transplant program here at U.Va. in the late ‘80s,” Kron said. “And we had a young guy. We did a transplant on and everything went perfectly, but this inflammation reaction caused the lung not to work at first … So, that’s how we got the idea of trying to treat this problem during lung transplantation.”
According to Lau, inflammation that occurs during lung transplantation surgeries is clinically defined as ischemia reperfusion injury. Removal and transportation of the donor lungs on ice causes ischemia — inadequate blood supply to an organ — which then requires reperfusing, restoring blood flow to the organs the recipient’s own blood that will create an injury to the lungs.
During reperfusion, the recipient blood entering the lungs tends to carry a large amount of white blood cells and other chemicals as a result of the body’s automatic inflammation reaction. This inflammation and surge of chemicals into the donor lungs causes an early injury to them, Kron said.
According to Kron and Lau, administering low-dose regadenoson into patients during transplantation will affect the A2A adenosine receptors — adenosine receptors on the tissues of the lung — ultimately reducing the number of white blood cells and other substances that can enter the lungs.
After receiving funding from the National Institutes of Health and approval from the Food and Drug Administration, Lau and Kron started testing this drug on humans November 2017.
Lau and Kron hope to finish the first stage of the trial — also known as a “safety trial” — within the next two years. Phase one is designed to safely administer this drug on 21 patients to determine the safest dosage for humans and ensure the drug is limiting reperfusion injury to the lungs.
Two people have successfully undergone lung transplants with regadenoson. The researchers are also determining the side effects of the drug during this safety trial. Regadenoson, as a vasodilator, can cause secondary reactions including headaches, dizziness and nausea, but as a lung transplant drug, has unknown side effects that are currently being studied.
“We hope it is safe for human beings, and then we will be able to move on and show that it really works because if we can reduce this reperfusion injury, it will make lung transplants safer,” Kron said.
According to Kron, a few years following transplant surgery, a patient may be diagnosed with bronchiolitis obliterans, a disease that induces a chronic rejection of transplanted lungs. This normally occurs five to ten years after transplantation, making the regadenoson treatment a short-term solution to tackle a reperfusion injury that occurs early after surgery.
“We believe what happens is the lungs get an early reperfusion injury that sets them up for later rejection,” Kron said. “If we wipe that out, maybe it will make lung transplants much better long-term therapy than it is right now.”
According to Lau, the current survival rate of a patient who received lung transplantation five years ago is 50 to 60 percent. She hopes this research study will improve the survival of lung transplant recipients.
In the future, Lau hopes to heal damaged lungs that can’t be donated by flushing these organs with high doses of regadenoson before surgery through ex vivo lung perfusion, a procedure using a machine that maintains the lungs prior to transplant. This procedure may reduce inflammation in imperfect lungs to improve their functionality and make them viable for transplants.