The Jefferson Health District Community Health Improvement Plan was released March 8. Organized by the MAPP2Health Leadership Council through the Virginia Department of Health, the plan identifies four priority areas for improvement in the next three years — promoting healthy eating and active living, addressing mental health and substance use, improving health disparities and access to care and fostering a healthy and connected community.
The plan was created using the Mobilizing for Action through Planning and Partnerships model developed by the Centers for Disease Control and Prevention and the National Association of City and County Health Officials. The model fosters collaboration between community stakeholders — including local leaders, hospitals and coalitions — to identify the most pressing health issues to be addressed.
Denise Bonds, District Director of the Thomas Jefferson Health District and Assoc. Prof. of Public Health Sciences, described the plan as a joint effort between agencies, the community, the health department and the two hospitals in the district — the Sentara Martha Jefferson Hospital and the University Medical Center.
Bonds played a central administrative role in the creation of the plan.
“I’m the health director for the district, so my staff members served on that core group,” Bonds said. “My role was to make sure we have staff — that development has a plan. We also will help with our other core members to run the annual reporters and provide the data.”
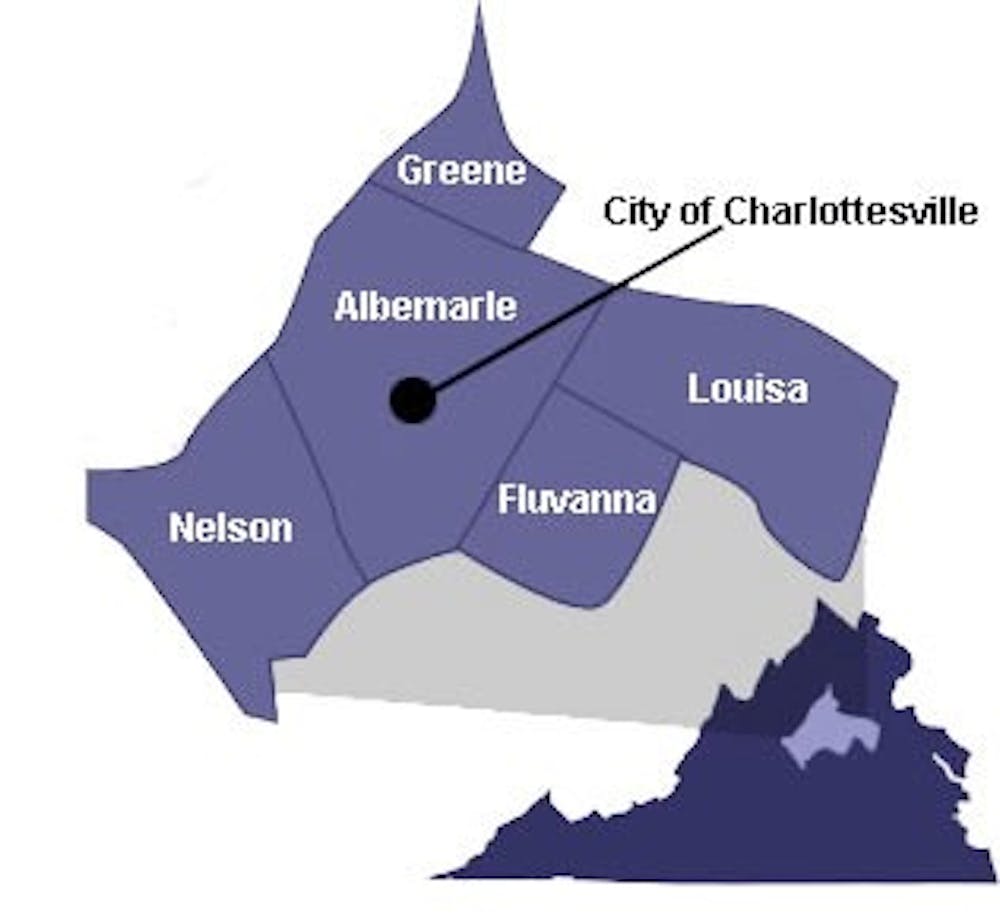
Bonds highlighted the University’s role in the Jefferson Health District, which includes the City of Charlottesville and Albemarle, Fluvanna, Greene, Louisa and Nelson counties.
“[The plan] belongs to everyone in our community,” Bonds said. “[University] students can join one of our coalitions, work on strategies to foster a health and connected community… [For example, University] students could help agencies by talking to high school students in our area about what a healthy relationship looks like.”
Peggy Whitehead, Executive Director of Blue Ridge Medical Center in Nelson County, said the improvement plan was in line with the medical center’s goals.
“I had a pretty intense interest in the outcome of the whole study, because Blue Ridge Medical Center is required to do a health needs assessment every three years,” Whitehead said. “When I get ready to do my submission in the coming August for our service area competition grant, I’ll be able to use the information that has been gathered.”
The information used to identify the four community priorities comes from a variety of sources, including online Center for Disease Control material, census information and hospital admissions data.
“There’s so many subjects that for months we were looking at data … And figuring out what we were most concerned about — so we can really take a deep dive into it — and discussing it with each of our perspectives as providers of health and human services,” Whitehead said.
The next step will be implementing the plan. Whitehead said they will discuss potential responses to the plan at a meeting scheduled for March 20.
“The health department would like to see each of the four initiatives … Have a champion, and so we need people from various agencies, whichever seems most appropriate, to champion progress and various steps that we might want to take to address the issues that have been identified,” Whitehead said.
The 2017 plan is the third plan created, with the most recent one released in 2012. Assoc. Prof. of Family Medicine M. Norman Oliver has been a part of all three plans.
“I participated with a number of individuals representing organizations in Charlottesville in helping to develop the four main strategic goals … And I’m really excited about this one because one of the goals is access to care and reducing health disparities across racial, ethnic and geographic categories,” Oliver said.
Oliver described the plan as a reflection of the concerns of the community.
“I think it underscores the fact that the only way you can really develop plans that are meaningful for communities is to have this interior sectoral collaboration from many different stakeholders,” Oliver said. “That certainly was the case for this, and now we have the job of actually implementing it, and that will take the same kind of partnership.”
While the Thomas Jefferson Health District is not alone in forming community-based health improvement plans, Oliver believes it does so exceptionally well.
“I believe what we are doing here is an example that’s going to be hopefully replicated in many health districts across the state,” Oliver said. “[And] it’s not just here in Virginia, but places all around the country.”