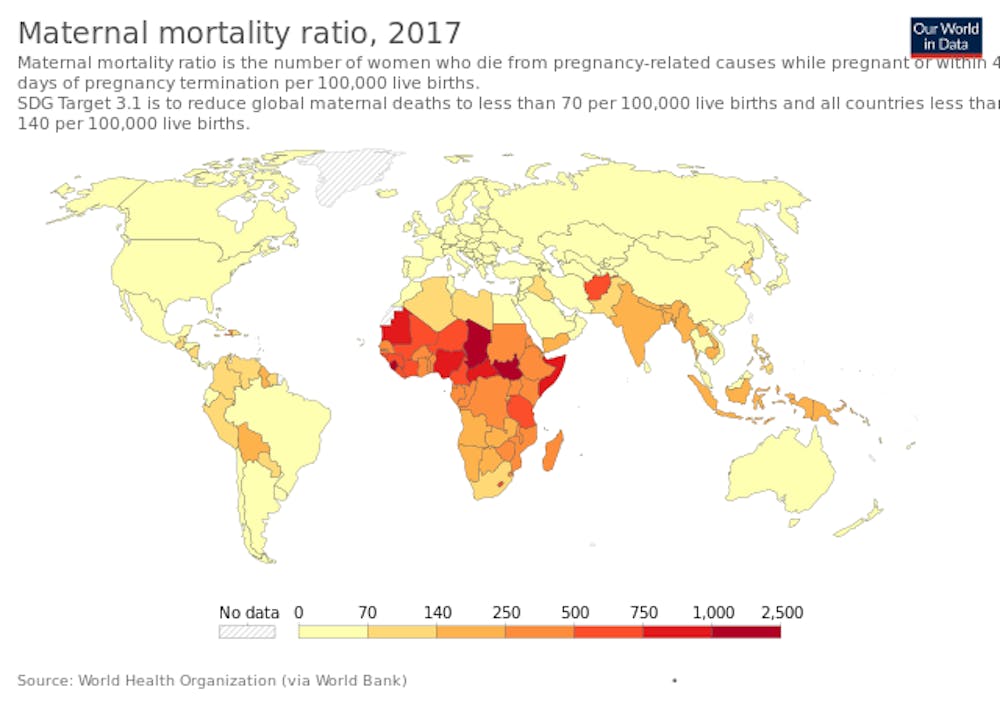
A ProPublica and NPR investigation found earlier this year that more American women are dying of pregnancy-related complications than women in any other developed country. The University Health System is working to mitigate this rising maternal risk with an approach that includes comprehensive screenings and emergency protocols.
Maternal mortality is most dangerous to mothers who carry high-risk pregnancies.
“High risk pregnancies are those in women whose pre-existing medical conditions can be negatively impacted by pregnancy,” said Chris Chisholm, an associate professor of obstetrics and gynecology and the vice-chair for medical education at the University Health System.
Pre-existing conditions are present in the mother before or surface during pregnancy and threaten the health of both the mother and the child, with the most common being cardiovascular and hemorrhage-related.
Maternal mortality and risk can even occur following a successful pregnancy and delivery.
“Pregnancy-associated mortality records count deaths occurring in the first year after pregnancy and include accidental and traumatic deaths, as well as suicide,” Chisholm said. “Unfortunately, a number of women die as a result of intimate partner violence each year.”
Postpartum depression is also a risk to mothers following pregnancy.
“Postpartum depression is the same as depression outside of pregnancy, and occurs in 10-20 percent of pregnant women after they have their babies,” said Donald Dudley, an obstetrics and gynecology professor and director of the Division of Maternal-Fetal Medicine.
The risk is in no way limited to those typically seen as at-risk.
“I had a physician colleague who committed suicide due to postpartum depression over 20 years ago, and it had a lasting impact on me,” Chisholm said.
The same NPR and ProPublica study found that the U.S. is the only developed country where maternal mortality is rising.
Dudley attributed multiple causes for this, including, “an older population becoming pregnant, more women with congenital heart disease coming into adulthood and getting pregnant, higher rates of obesity, de-regionalization of healthcare and improved detection.”
Both doctors praised the University Health System’s commitment to maternal health. The system’s Children’s Hospital programs include both neonatal and pediatric intensive care units and are nationally ranked.
“We are ranked in the top one percent of labor and delivery units in the country as a safe place to deliver,” Dudley said.
Chisholm spoke of multiple safety protocols, such as emergency drills and treatment protocols for hypertension, in place at the University Health System.
“All women are screened in pregnancy for intimate partner violence, substance abuse and depression. Women are screened for medical risk factors which are managed throughout the pregnancy,” Chisholm said.
Dudley also spoke about the University’s high quality of care.
“We have some of the best nursing staff around and a great group of obstetricians and midwives, along with all of the subspecialty care a pregnant woman could possibly need,” Dudley said. “The goal at U.Va. is be the safest place to deliver your baby in the world.”