An April 2019 study by the lab of University Assoc. Biology Prof. Sarah Kucenas has recently discovered a novel way that cells of the peripheral nervous system can be repaired following damage. Post-doctoral fellow Laura Fontenas and fourth-year College student Melanie Piller collaborated with Kucenas on this study.
This project was already being researched when Piller and Fontenas joined the lab in 2015 and 2016. The lab team ultimately discovered that damaged PNS cells can be restored with the help of a type of cell that usually resides in the central nervous system, an oligodendrocyte.
Oligodendrocytes are a type of cell in the central nervous system, found mainly in the spinal cord. Their main job is to form myelin, a protective and insulating layer that increases the speed of electrical impulses along neurons.
When the myelin layer breaks down — due to reasons such as genetic mutations or disease — the speed at which the body’s nerve cells can communicate with each other severely slows. This can eventually cause pain, much slower movement and function, muscle atrophy and loss of fine motor skills. When this happens in the body, diseases such as multiple sclerosis, Charcot-Marie-Tooth disease or Guillain-Barre syndrome can result.
However, the oligodendrocytes typically remain in the central nervous system and do not migrate to the periphery. This causes a dilemma when the myelin of cells in the extremities becomes damaged.
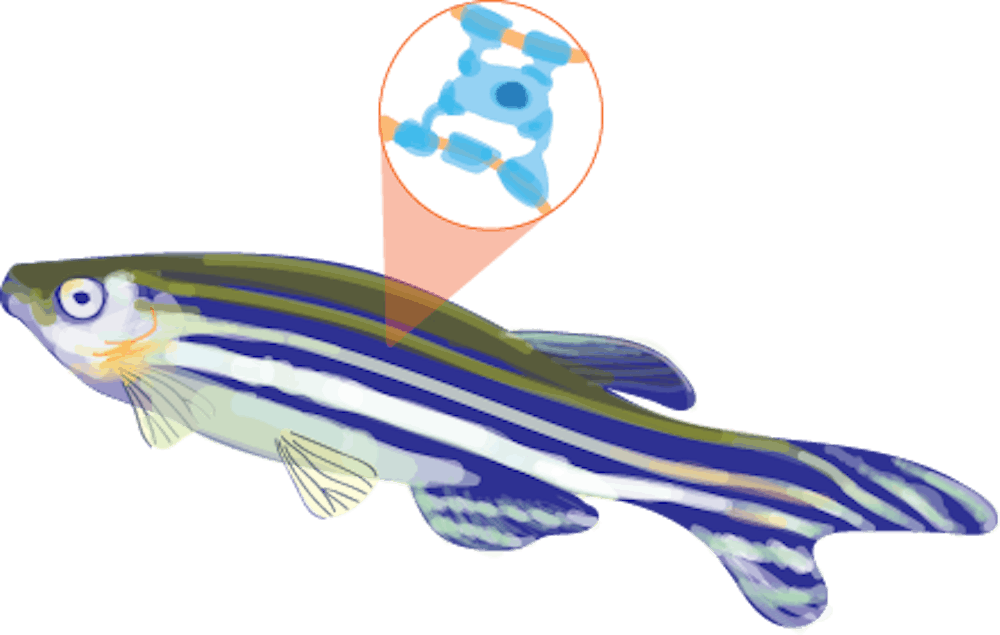
The lab approached the problem of myelin decay in the human PNS with a focus on the physiology of another organism. Piller explained that the lab chose zebrafish for a of couple reasons — its body is transparent during development and a majority of genes causing disease in humans have a counterpart of similar function in fish. Both of these aspects of the zebrafish contribute to an easier experimental design.
“We can use fluorescent markers and microscopes to watch development at the cellular level,” Piller said.
A specific advantage in research also stemmed from the transparency of the fish, which allows researchers to see the movement of cells around the motor exit point, or the boundary between the central and peripheral nervous systems. CNS oligodendrocytes had previously been thought to not migrate to the other side.
“And because of their small size, we can image both the central and peripheral nervous systems at the same time and observe glial cells cross the MEP transition zone in real time,” Fontenas said.
The unusual movement is caused by a compound that disturbs normal nervous system functions so as to pull oligodendrocytes into the peripheral region. This was performed on zebrafish that had been genetically modified to show symptoms of diseases that deal with the breakdown of myelin. This way, researchers could study the effect of oligodendrocyte movement across the transition zone and see how the cells repaired myelin layers outside of their normal region.
The study has brought to light a mechanism that was previously thought to be highly unusual if it occurred at all.
“We showed that oligodendrocytes can exit the spinal cord to reach the peripheral nervous system and that they are able to myelinate motor nerve axons in a hypomyelination model,” said Fontenas. “These results are encouraging cause we now know that oligodendrocytes can migrate to and function in the peripheral nervous system.”
This research has changed the idea of oligodendrocytes as strictly CNS cells, widening both the understanding of their function and possible opportunities for their use.
Their findings may have important implications in how diseases affecting the myelin sheath are approached in future treatments.
“Currently, our knowledge of these processes is limited, but I hope our findings will help further the research in the field,” Piller said. “Eventually, this type of research could lead to new therapies for demyelinating diseases like Charcot-Marie-Tooth Disease and Multiple Sclerosis.”