The University reported its first case of COVID-19 Monday, but the University Health System has been developing plans to treat COVID-19 patients since February. A diverse team of doctors, scientists and hospital administers have created an action plan that involves screening clinics, overflow spaces and specially reserved intensive care unit rooms to effectively treat patients. As more COVID-19 cases arise in the United States and Virginia, the University Health System is implementing more and more of its action plan.
Chris Holstege, executive director of Student Health, and Costi Sifri, director of hospital epidemiology in the University Health System, are leading the initiative to fight COVID-19.
William Petri — medical professor and vice chair for research, who specializes in immunology — addressed the extent to which the health system has prepared.
“There are reserved ICU rooms,” Petri said. “We have made a new COVID-19 screening clinic in the Battle building. We also have additional overflow spaces prepared all throughout the health system.”
New guidelines have been put in place for the standard hospital and health system operations. All ambulatory clinic visits — outpatient medical care for routine and specialty consultation, diagnosis, observation and rehabilitation — between now and April 6 are to be rescheduled for a later date. Urgent care and sick visits will still be held.

The University's COVID-19 test currently has a turnaround time of less than 24 hours.
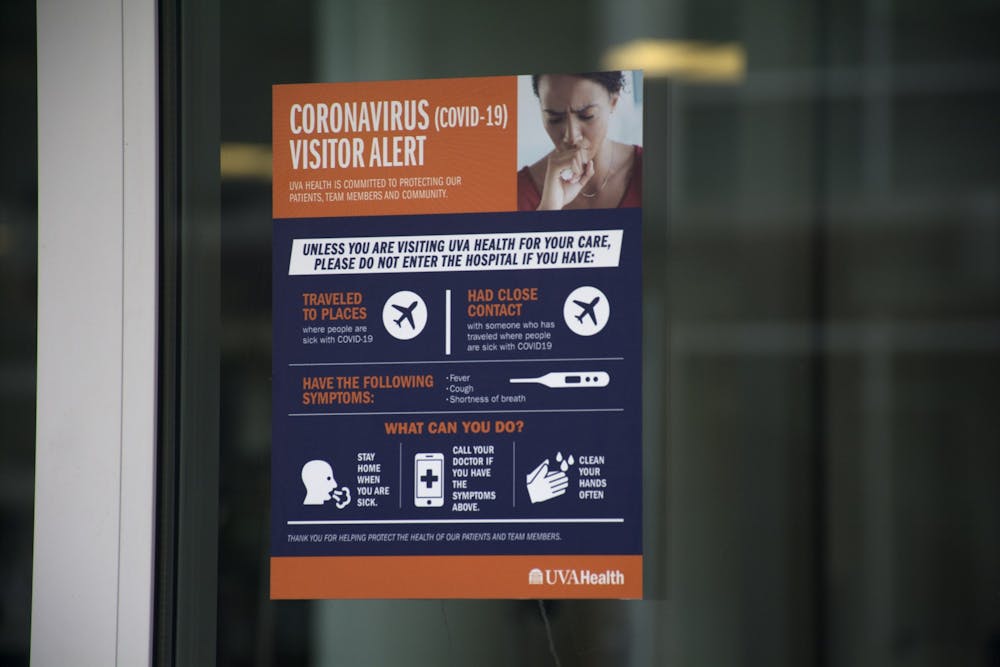
In addition, all hospital visitors must be screened for respiratory symptoms and possible COVID-19 exposure before visiting patients, and patients are limited to two visitors ages 18 and older during their stay at the University hospital. Children under 18 are not allowed as visitors during this time.
Despite the planning and guidelines, there are still challenges operating under the pandemic, according to Petri.
Tests for COVID-19 must first travel to Richmond for processing before results can be obtained, which can take several days, though the health system hopes to have all testing steps local within the coming days.
Tracey Hoke, chief of quality and performance improvement in the health system, further clarified the testing status.
“We are moving now towards three new platforms that will offer us some in-house testing,” Hoke said. “The first platform is low [sample volume] — one where not too many samples can go in — so we won’t have a lot of tests with this, but with it, we will soon have options for in-house testing.”
Cirle Warren, associate professor of medicine in infectious diseases, explained the important testing guidelines that the health system is following in an email to The Cavalier Daily.
Those with a fever, cough, difficulty breathing or flu-like symptoms should first call their primary care physicians to see if testing is needed, according to Warren. For now, only individuals in two scenarios are prioritized for testing — those who have travelled to areas where there is a widespread, ongoing transmission of COVID-19 as defined by the Centers for Disease Control and Prevention, including but not limited to China, South Korea and the United Kingdom, and those with severe symptoms that cannot be explained by other viruses.
Hoke believes the University’s first case of COVID-19, a Maxine Platzer-Lynn Women’s Center employee, was treated through her primary care physician and tested through LabCorp — a private lab testing company — as she was not seen or treated by the University Health System.
Hoke also confirmed the health system’s preparedness for challenges posed by COVID-19, like complications disrupting trade and travel to Asian countries and school closures creating staffing issues if hospital employees cannot find childcare.
“This isn’t the first time a pandemic has come around in healthcare, and we have a plan and [a] group in place for caring for patients who need to be hospitalized,” Hoke said. “We’ve also made plans for the staffing of [the health system] and plans to preserve our protective equipments, which many are made in China and [other Asian countries].”
However, for those without severe symptoms, both Petri and Hoke agree that the best plan is perhaps the simplest — staying home, calling their primary care physician if necessary and practicing social distancing.
They encouraged people to follow the CDC’s guidelines, such as those to avoid events with more than 10 people. These practices are especially important because the virus is unusually contagious and often presents with no symptoms for days on end, during which individuals can infect others.
Petri traces the virus’s contagiousness to humans’ lack of immunity and calls for social distancing as the only way to slow the pandemic.
“What’s different about this coronavirus is that people don't have immunity,” Petri said. “It has jumped from animals into people.”
According to Petri, the virus changed when it traveled from a bat into humans — leading to an entirely different virus for which humans do not possess immunity.
“If left unchecked, half the population [of] the U.S. will get infected because we don't have a pre-existing immunity,” Petri said. “The whole idea is slowing down the epidemic so we don't overwhelm hospitals because we have limited capacity.”
Hoke also emphasized the importance of social distancing to prevent shortages of medical supplies and hospital beds.
“If patients are not very sick, they should stay at home and call their primary care providers so [as to] not flood the healthcare system,” Hoke said. “The idea of flattening the curve, or lengthening the time it takes for COVID-19 to reach people in the community, is very important.”
The University Health System is consistently monitoring COVID-19 outbreaks in Virginia and the United States. The most recent updates, information, policies and contact numbers can be found on its website. Additionally, the CDC provides COVID-19 information for businesses, employers, schools, childcare and community and faith-based organizations — as well as information for individuals and families. For the most recent action plan, see the President’s Coronavirus Guidelines for America: 15 Days to Slow the Spread.