The U.Va. Biocomplexity Institute’s COVID-19 model predicts a peak in COVID-19 cases in Virginia in February if the cold weather or new variants continue to increase case growth. Based on current trends as of Jan. 7, these circumstances may cause new cases in Virginia to peak at around 57,000 per week during the week leading up to Feb. 21. If additional measures are taken to control the spread, however, new cases may peak at around 30,000 per week leading up to Jan. 10.
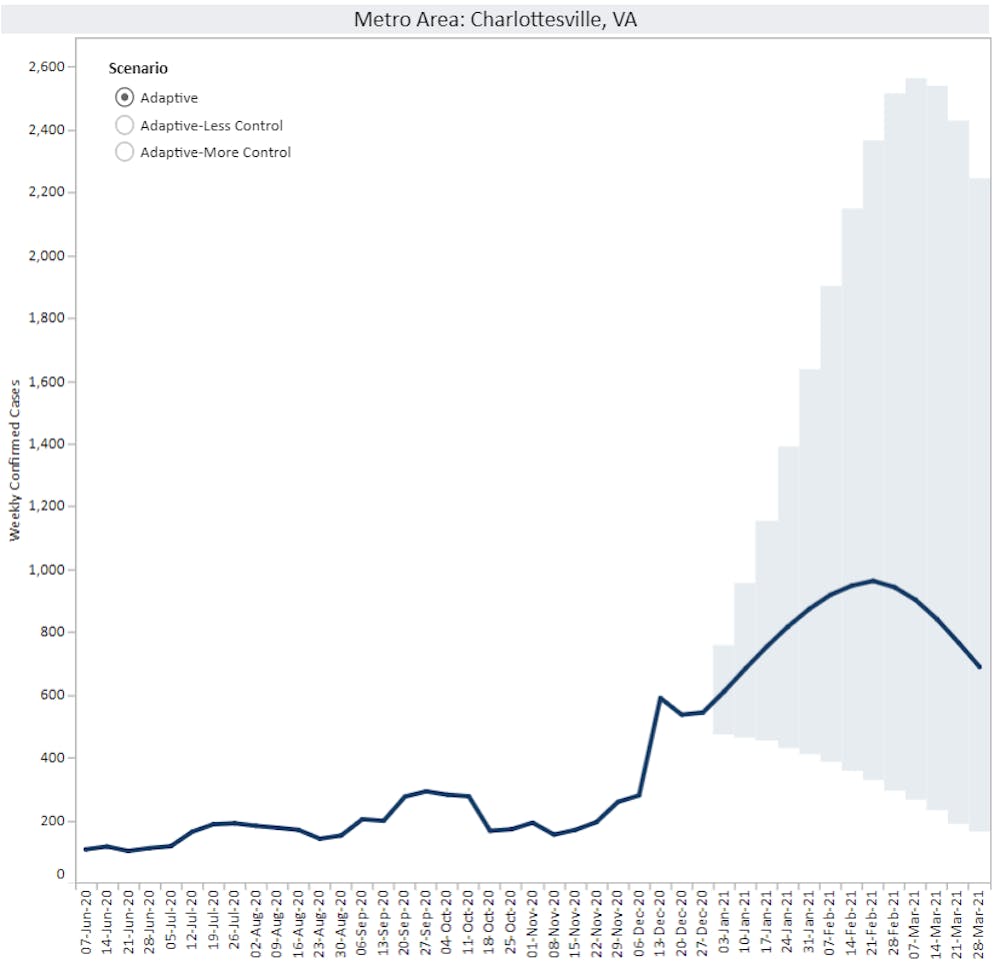
In Charlottesville, new cases may peak at around 2,000 per week leading up to Feb. 28 under conditions of less control. If there is more control over the virus, cases may peak at around 800 per week during the week ending Jan. 17. In Virginia, statewide COVID-19 restrictions were implemented by Gov. Ralph Northam in an attempt to reduce the spread of the virus. These restrictions, which went into effect Dec. 14, include a modified stay at home order, a universal mask requirement and a limit of 10 individuals for social gatherings.
The predicted peak in February means that students may be returning to classes in Charlottesville during a period of increasing COVID-19 cases in Charlottesville and throughout the state of Virginia.
The Biocomplexity Institute provides weekly updates to the University regarding the course of the virus, helping to shape the University’s COVID-19 decisions and policies. The model is updated weekly and is currently in its 42nd week of continuous updates.
“University public health experts are constantly monitoring a range of variables and metrics with respect to the coronavirus pandemic,” University Spokesperson Brian Coy said. “The Biocomplexity Institute’s COVID-19 model is certainly one of the sources of information they monitor, as well as other relevant models and the current data about the progression of the virus in the region, in Virginia, and around the country.”
The Biocomplexity Institute has worked with infectious disease models for over 20 years, providing support and responses to Zika, Ebola, Influenza and other epidemics. A team of around 80 people — including members of the Biocomplexity Institute, University faculty and partners from other institutions — began working on a COVID-19 model in February of last year.
The model is the leading one of its kind in Virginia, used by state and county governments to monitor the potential spread of the disease and modify policies accordingly.
According to Madhav Marathe, division director and distinguished professor in biocomplexity at the Biocomplexity Institute, the projected peak in February is due to a variety of factors — the surge in cases during Thanksgiving and winter break, cold weather leading to more indoor gatherings, concern for businesses and a general sense of COVID-19 fatigue as some people become tired of social distancing policies.
Marathe, however, emphasized the importance of working collectively in order to reduce the impact of the virus. He believes that if people continue to follow health guidelines and decide that this is something they collectively want to take care of, the problem should not be hard to resolve.
“The disease is still very much under our control,” Marathe said. “When we all come together and work as a team, we can control this [outbreak], but we have to work collectively. It’s not enough for one small county to control it and others not to control it … It’s not good enough for just a state to control it and not other states to control it.”
According to Marathe, projections are not made beyond a couple of weeks because the disease dynamics are intimately tied to people’s behaviors and perceptions of the disease. As a result, these projections are generally not referred to as forecasts because of their constant potential for variability.
Unlike weather forecasts, where the projected weather does not impact what actually happens, epidemic models make projections that are endogenous to the system, meaning that the projection affects the result. Consequently, the dynamics of the epidemic change with people’s behaviors.
“The disease goes in a particular direction, we all perceive the disease, that perception leads us to changing our behavior one way or the other, and the policies might change,” Marathe said. “That in turn changes where the disease goes. There’s a constant loop where people are changing their behavior constantly as they perceive the disease.”
Vaccines have also been taken into account in the model. However, while it is expected for vaccines to reduce new case growth in the long run, for a while there may be an increase in cases due to a false perception that getting vaccinated means normal activities can immediately resume.
Beyond the Virginia model, the Biocomplexity Institute has a university campus model that is a digital replica of Grounds and calculates the odds of virus transmission at the University. By using anonymized student schedules and student IDs, the model tracks which buildings students frequently travel to for class and where they tend to interact with others, including other actions such as grabbing lunch or going to the library within the data as well.
The model is trained using numbers from the University’s COVID-19 tracker and is based on a PatchSim model which has been used in county-level COVID-19 forecasting.
“These kinds of models, the way that we use them is for short-term projections and these alternative realities, comparing counterfactuals,” Research Associate Professor Bryan Lewis said. “If we’re in a world where we make this decision, this is how the disease may behave. If we’re in a world where we just keep doing what we’re doing, this is how the disease may behave.”
The model is driven by contact rate parameters — a time varying parameter governing PatchSim model outcomes that is a function of the transmissibility of the disease and the rate at which susceptible individuals come in contact with infected individuals. To predict future cases, possible contact rate values are assumed. Three scenarios are created — one where the contact rate either remains the same, indicating the amount of interactions remaining the same; one where the contact rate is doubled, indicating an increase in interactions; and one where the contact rate is halved, indicatings a decrease in interactions.
A 14-day forecast of campus cases, including confidence intervals, are sent to the University on a weekly basis. According to Aniruddha Adiga, postdoctoral research associate at the Biocomplexity Institute, the models initially overpredicted the number of cases, but as more data became available, they became more accurate. The confidence intervals are narrow, with the true values mostly falling within the forecasts’ confidence intervals.
The model stopped being updated after Thanksgiving Break due to a shortage of data, with most students leaving Grounds.
“It’s very hard to make our predictions with just a handful of numbers — you cannot rely on the accuracy of the model,” Adiga said. “Hopefully when the campus reopens, we’ll be restarting our predictions, and hopefully this time we’ll be having [even] more accurate data.”
Currently, the University is still on track to welcome students back to Grounds for the first day of classes on Feb 1. Any changes in plans will be announced by Jan. 15.
The Biocomplexity Institute will resume their weekly updates to the University on Feb. 1 with the start of the spring semester.