In an effort to manage increasing COVID-19 hospitalizations, U.Va. Health instituted a new policy mandating that all registered nurses, certified nursing assistants and patient care technicians in inpatient units pick up an additional 12-hour red shift — one that has a high need for additional staffing — every three weeks. The policy went into effect Jan. 10.
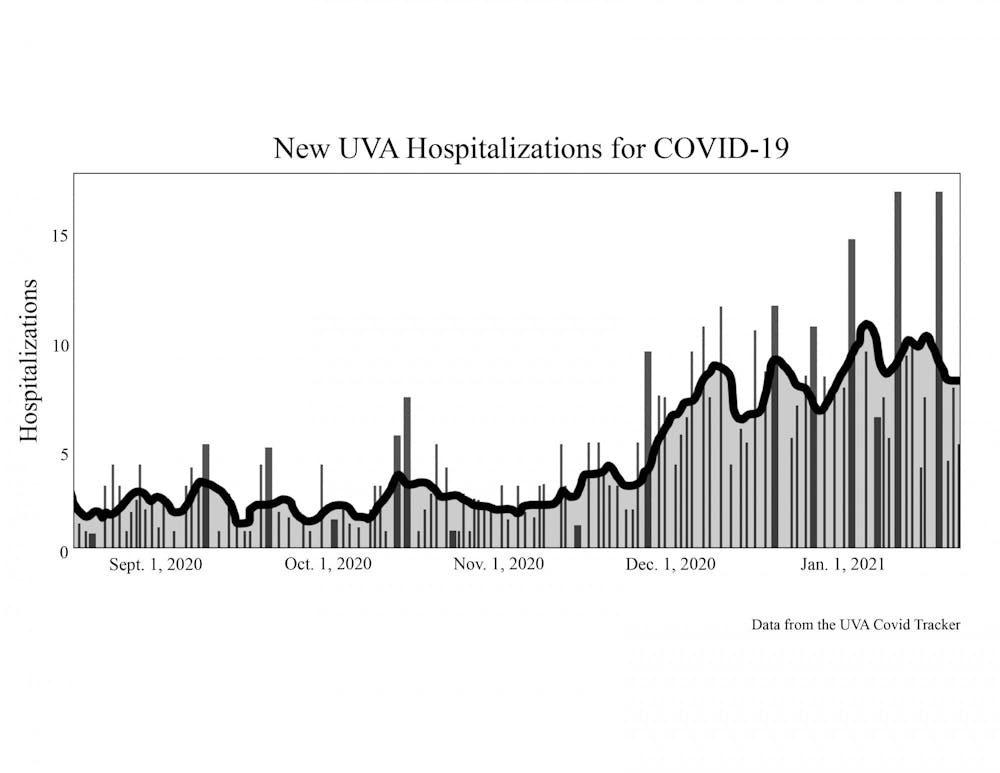
U.Va. Health saw a surge in hospitalizations following Thanksgiving break, and the number is anticipated to continue rising over the course of the next six weeks. As of Tuesday, there were 55 hospitalized COVID-19 patients at U.Va. Health. There were 9 new COVID-19 patients admitted to U.Va. Health on Tuesday. On Jan. 20, 16 new COVID-19 patients were admitted to U.Va. Health, the highest number of new admissions in a single day since the University’s COVID-19 tracker began reporting statistics on Aug. 17. The current seven-day moving average is 8.43 hospitalizations, compared with a seven-day average of 3 hospitalizations in August.
According to the CDC’s ensemble hospitalizations forecast based on data from 13 modeling groups, COVID-19 hospitalizations in Virginia are expected to increase in the weeks leading up to Feb. 15. Nationally, the number of new COVID-19 hospital admissions predicted to be reported on Feb. 15 ranges from 9,300 to 21,000.
To protect the health of patients and hospital workers amidst increasing COVID-19 hospitalizations, U.Va. Health barred visitors beginning Jan. 13. Special exceptions can be made for specific patients such as pediatric patients, patients with disabilities and patients at the end of their lives. However, visitors can not have COVID-19 or symptoms of any other infectious diseases and are screened prior to entering the hospital. These visitation restrictions are similar to those implemented in March 2020 when the pandemic was in its early stages.
The hospital previously had to turn away some patients, referring them to other hospitals, due to many staff members being reallocated to COVID-19 patients. According to Eric Swensen, U.Va. Health Public Information Officer, the hospital continues to care for all patients coming to the Emergency Department and accepts transfers from other hospitals as beds become available.
“We continue to make these adjustments on a daily basis as our COVID care needs change rapidly,” Swensen said.
Previously, many staff members had already voluntarily picked up extra shifts for incentive pay, but further projected increases in hospitalizations have led to an additional need for support. During these shifts, registered nurses will receive an additional $20 per hour, while certified nurses and patient care technicians will each receive an additional $10 per hour.
For staff members who are unable to pick up extra shifts, other staff members can fulfill this requirement in their place once they have completed their own requirement. Staff members who have previously picked up incentive shifts are not required to pick up more.
U.Va. Health CEO Wendy Horton and Chief Nursing Officer Mary Dixon are both hopeful that the expectation can be removed around six to eight weeks after the policy was originally instituted, but it all depends on COVID-19 volumes. The hospitalization rate is anticipated to increase within that time period.
“We don’t know how dramatically it will rise but we want to be able to have the resources available and the teams available to be able to provide that level of care and to maintain a constant culture of safety for our patients, but also safety for our team members,” Dixon said. “When our team members don’t necessarily have the complement of the team that they need to meet the needs of our patients, that’s not the environment that we want any of our team members to be working in.”
U.Va. Health focuses on three primary areas in terms of managing the hospital during the pandemic — the amount of available equipment, beds and staff. COVID-19 patients are generally housed in Special Pathogens Units — which were developed in spring 2020 to separate patients that have COVID-19 from those who don’t — but once patients reach the point when they are no longer infectious, they can be moved to other medical-surgical intensive care units or acute units so that the needs of newly diagnosed infectious patients can be met. While they still require care and hospitalization, they can be treated as non-COVID patients and housed in non-COVID units to create additional space.
The hospital currently has adequate equipment and beds, but the area that they are monitoring most closely is their workforce, which Horton described as their “rate-limiting step.”
“Everyday we need to make fine-tune adjustments in how we’re staffing, how many patients we can take and what that looks like,” Horton said. “It’s a very dynamic process and something that a whole team of people meet about and talk about to make sure that we’re on top of things and monitoring things and ensuring the safety and quality of our patients and all of our team members that work here.”
U.Va. Health workers recently unionized due to reasons including inadequate staffing, top-down management and subpar wages. Especially during the pandemic, hospital workers have faced increased stress regarding their own wellbeing as well as the wellbeing of their patients in an already high-paced and stressful workplace.
Julie Brylawski, a Nursing student and patient care technician at U.Va. Health, mentioned that their department used to require working one 12-hour shift as a baseline requirement per pay period, which is every two weeks, but around October, the requirement rose to two shifts per pay period on average. This new policy only adds on to previous requirements. According to the student, the reality is that many employees have gotten sick, experienced burnout and quit.
“We need the staff, and I think we all can identify that having a few more people every single shift makes our lives a lot easier, but if that means every single person is working overtime, does that really improve patient care?” Brylawski said. “Does it improve patient outcomes if everyone’s exhausted? I don’t know.”
Personally, because she works for a more flexible department, she is not as outraged by the policy, but she wonders how people with other responsibilities can manage and how the situation might change when classes begin.
The hospital has worked to support their team members during this difficult time and implemented incentive pay as a way of thanking them for the extra time they are committing to their patients. Additionally, the hospital has a program on wellbeing and wisdom with several resources available to team members. Dixon said that the hospital was trying to do things at both the unit and system levels in order to “support the resilience and the stamina of our team.”
“Our team members go through different periods individually of being tired,” Dixon said. “This is not easy work. This is probably one of the most challenging periods in healthcare for anyone who’s in healthcare — be it a nurse, be it a physician, be it an administrator — to help us care for our patients and make all the right decisions.”
A CNA and nursing student at a nearby community college — who asked to remain anonymous because they didn’t want what they said to impact their work — feels that the hospital has been very supportive of students. In their department, the minimum hour requirement for students is one 12-hour shift per week while for non-students, it’s two 12-hour shifts per week. They were previously scheduled like a regular employee because they wanted to help, but when it became clear that their school and work schedules were not compatible, their supervisor was able to bring them back to their minimum hour requirement.
“Prior to that, if they had held me to my original schedule, it would have been very stressful to the point that I think my studies would be in jeopardy,” the second student said.
Due to a medical exemption, the anonymous CNA is unable to work with COVID-19 positive patients, but they nevertheless have to pick up additional red shifts in non-COVID-19 units. However, they said they still feel safe in their current work environment at the hospital. People have been protective of them on every unit they’ve been on, and they feel that the hospital’s PPE and testing policies are good.
“If there’s any shadow of a doubt that someone is [a patient under investigation for COVID-19] or even combative, they’ve really put my safety first,” the CNA said. “Whenever I’ve spoken up about something that I’m not comfortable with, I have been accommodated and they have worked with me. I feel safer at the hospital than I do at the grocery store. But I think I’m lucky.”
Horton emphasized that vaccinations, social distancing, mask wearing and hand washing will continue to be key moving forward. Despite many people feeling fatigued, she believes that these actions really are the answer.
“We’re pretty excited about the future, and we just ask everyone to continue their great work,” Horton said. “When everyone continues doing their part, it really is supporting all of us. We just want to say thank you for that support because when people do all the right things, it really helps the healthcare system as well.”