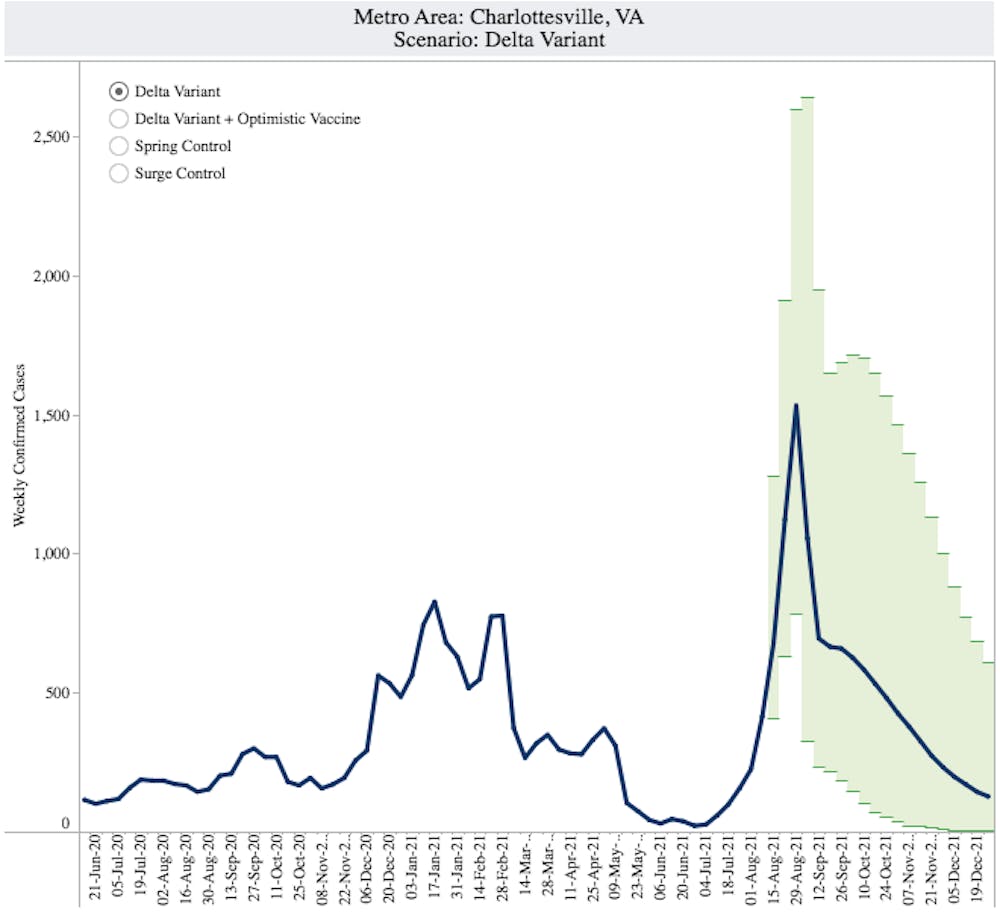
If the Delta variant continues its current trajectory and behaviors do not change, Charlottesville could see a peak in cases during the week ending Aug. 29 — the first week of classes for undergraduate students.
The University Biocomplexity Institute’s COVID-19 model predicts a potential peak of 1,531 weekly cases in what could be the greatest spike in cases in Charlottesville since February, when over 750 cases were recorded within a single week. Statewide, the peak may come a few weeks later during the week ending Sept. 12, with a potential high of 72,031 cases.
According to Madhav Marathe — division director and distinguished professor in biocomplexity at the Biocomplexity Institute — these projections are not forecasts, but possibilities that are subject to change depending on evolving human behaviors and attitudes towards the virus.
The model lays out four different potential scenarios from worst to best — Delta variant where there are no interventions and the virus continues its spread as is, Delta variant plus optimistic vaccine where there are higher rates of vaccination, surge control where increased control from non-pharmaceutical interventions like mask-wearing reduce transmission by 25 percent and spring control where vaccination levels remain the same but cases return to the lowest levels seen in the spring.
“[Spring control] seems to be very hard to achieve now,” Marathe said. “Doable, but hard, because, in fact, schools are opening, fall is coming, so more indoor activities are going to begin … those things make it harder to go back to spring levels.”
Following the peaks in January and February, cases in Charlottesville began to decline for the remainder of the spring semester. During the week of March 14, 265 positive COVID-19 cases were recorded, the lowest weekly case count since December. Numbers further dropped from May through July as schools closed and students headed home for the summer.
Graphically, there are minimal differences between the Delta variant and the Delta variant plus optimistic vaccine scenarios because the vaccination rate in Virginia is already quite high, with 55.3 percent of the population fully vaccinated. In the Blue Ridge Health District, 62.9 percent of the population has received at least one dose of the vaccine, while 57.3 percent of people are fully vaccinated. Nevertheless, increased vaccination rates will still help to lessen the peak.
The projected peak under both scenarios, however, is higher than the January peak. Charlottesville’s last peak was during the week ending Jan. 17, when there were 826 weekly cases compared to the potential new peak of 1,531 cases during the week ending Aug. 29 if no new measures are taken to quell the spread.
Despite these possibilities, Marathe said he did not believe the Delta variant or Delta variant plus optimistic vaccine scenarios would occur because “people will change,” but the difficulty with these projections comes with the fact that “how they might change is not easy to predict.” Case numbers might vary from county to county depending on different attitudes towards mask-wearing and other preventative measures.
“The fact that this can even be a possibility based on the models is a worrisome issue,” Marathe said. “I don’t think that this will happen unless we all completely just give up in some way, which is unlikely in Charlottesville ... but it all depends on how people behave.”
The one silver lining, according to Marathe and a weekly report from the Biocomplexity Institute, is that while the Delta variant is more likely to cause hospitalizations and prolonged illness, vaccines are effective in preventing severe illness and hospitalization and produce a stronger antibody response than in those who have previously been infected. That means that hospitalizations and deaths may not increase in proportion to the rising number of cases if more people become vaccinated.
According to the University’s COVID-19 dashboard, 37 individuals are currently hospitalized for COVID-19 at U.Va. Health, six of whom were admitted Tuesday. During the peak in cases in January, U.Va. Health saw its greatest number of single-day COVID-19 hospitalizations, with 16 individuals hospitalized on both Jan. 13 and Jan. 20. On Jan. 16, there were 61 total individuals hospitalized for COVID-19. The surge in hospitalizations led to U.Va. Health requiring nursing staff to pick up extra shifts.
Move-in for first-year students began Wednesday, and classes are scheduled to begin Aug. 24. According to Srini Venkatramanan, research scientist at the Biocomplexity Institute, the current model is driven by community case rates and does not incorporate the potential effects of student move-in or in-person classes.
“In terms of overall projected peaks, some of our updates in the December-January time frame did have higher estimates [than current projections],” Srini said. “It is to be noted that while some of it was due to seasonal effects and the largely unvaccinated population, the current surge is driven by the more transmissible Delta variant.”
The now-dominant Delta strain of the coronavirus is present in all health regions of Virginia and makes up about 80 percent of COVID-19 cases in the state. First reported in India, the Delta variant is more contagious than other strands of the virus. Thirty-three of Virginia's 35 health districts are experiencing a surge in cases, with the other two experiencing slow growth. The Virginia Department of Health recorded 2,552 new cases Wednesday while the Blue Ridge Health District recorded 49.
Despite having a similar vaccination rate to Virginia, Florida already exceeded its highest weekly case rate in the winter. University models are predicting that Virginia will follow suit and experience a massive surge in the upcoming weeks, with weekly incidence already up by almost four times that in mid-July.
The University has required all students living and learning on Grounds to get vaccinated, while those with vaccine exemptions must complete pre-arrival testing and be tested weekly. Faculty and staff are strongly encouraged — though not required — to get vaccinated. All individuals, regardless of vaccination status, must also wear masks when indoors on University property, though administrators are hoping to review the policy by Sept. 6.
Changing behaviors, however, can have a significant impact on the course of the virus. In January, the Biocomplexity Institute’s COVID-19 model predicted that cases would peak in Charlottesville in February under conditions of less control, with 2,000 weekly cases. Instead, the peak came with around 800 cases during the week ending Jan. 17, which is exactly what the model had predicted might happen under conditions of more control.
“What the final peak is really depends on our final actions,” Marathe said.