A recent discovery by researchers in the School of Medicine suggests a potential new target for osteoporosis and bone loss from rheumatoid arthritis. These findings explain why bone cells called osteoclasts tend to break down more bone than the body can replace.
Dr. Sanja Arandjelovic, assistant professor of nephrology at the U.Va. Carter Immunology Center, and Dr. Kodi Ravichandran, professor of microbiology, immunology and cancer biology, have helped to identify ELMO1 as a “signaling node” that regulates the activity of osteoclasts. The newly identified factors in this research could serve as pathways for therapeutic approaches.
The unexpected bone loss from osteoporosis — which afflicts nearly 200 million people globally — can lead to fractures in elderly women and men. Osteoporosis is also a condition associated with autoimmune disorders such as rheumatoid arthritis, an autoimmune and inflammatory disease in which the immune system attacks healthy cells by mistake. More than one million people in the U.S. suffer from rheumatoid arthritis, with bone loss affecting approximately one percent of those with RA. Thus, a better understanding of the causes of osteoporosis and ways to mitigate bone loss could have profound benefits to older patients and those with rheumatoid arthritis.
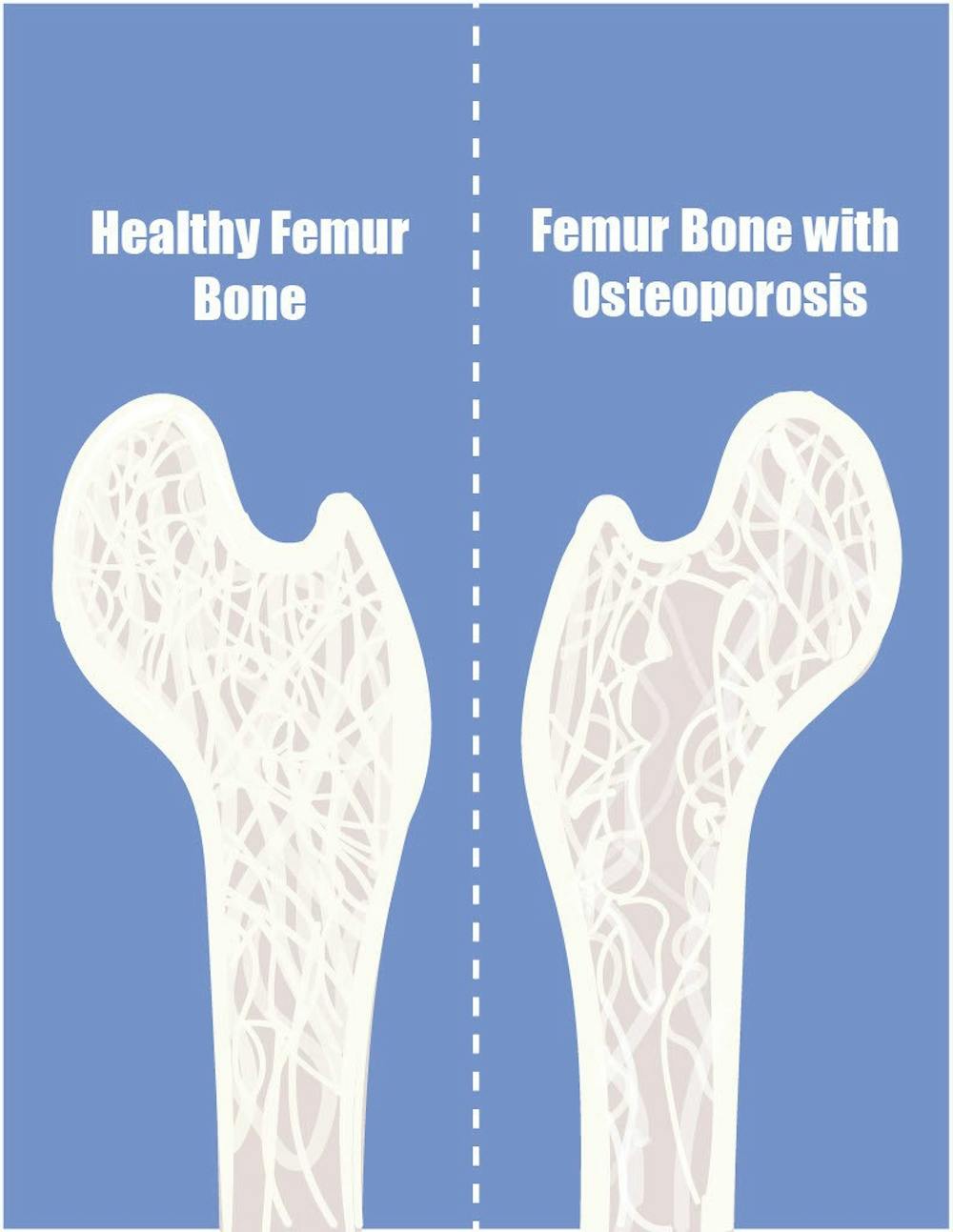
“Low bone mass is a precursor for the development of osteoporosis, a disease in which the bones become porous and weak and are prone to frequent breaks,” Arandjelovic said in an email statement to The Cavalier Daily.
Arandjelovic noted that per the Centers for Disease Control and Prevention, low bone mass is observed in more than 50 percent of women and 30 percent of men over the age of 50, with about 10 million people per year diagnosed with osteoporosis in the U.S. alone.”
In the setting of bone loss, osteoclasts are cells that help to break down or eliminate bone matrix, part of the bone tissue and forms most of the bone mass. Osteoblasts are cells that help to build new bone or repair fractured bone. Throughout life, the balance between osteoclasts and osteoblasts requires appropriate regulation. In pathologic entities, such as osteoporosis or rheumatoid arthritis, this balance is thrown off.
Arandjelovic said associations between bone disease and mutations in the gene called ELMO1 were observed and researchers discovered that the deletion of this gene could prevent osteoporosis in mice.
“We also found that inhibition of ELMO1 in cultured osteoclasts, cells that degrade bone, dramatically reduces their activity and bone loss,” Arandjelovic said.
In work published in the scientific journal Nature Communication, investigators blocked ELMO1 in two distinct RA preclinical models. By using a three-dimensional structure inhibitory targeted approach for regulating osteoclasts through the ELMO1 signaling pathway, the researchers were able to impede the degradation of bone matrix by osteoclasts. These findings may allow for new ways to regulate bone loss for patients afflicted by rheumatoid arthritis and, more broadly, osteoporosis.
Arandjelovic’s research has significant implications for the treatment of osteoporosis. The researchers succeeded in preventing bone loss in mice by blocking ELMO1 as well as for two different models of rheumatoid arthritis, suggesting that clinicians could prevent bone loss from osteoporosis and RA in people.
“Since ELMO1 deficient mice are overall healthy, our findings suggest that ELMO1 could be targeted for the development of new therapies to treat osteoporosis,” Arandjelovic said.